By: Mehroz Baig
Ron, a 79-year-old Bronx man, remembers the day a CAT scan revealed something was seriously wrong with his health.
“While the tech was doing the scan, she had this look on her face,” he said. “She said, ‘excuse me,’ and went and got the doctor.” The scan eventually showed he had developed pancreatic cancer.
Ron asked for his last name to be withheld because he hasn’t told much of his family or his friends that he was diagnosed with pancreatic cancer in August 2010 and he doesn’t want them to worry.
Ron is a small figure who walks fast wearing a white, short-brimmed hat covering a head of light gray hair and a black sports jacket. His health has put many restraints on his life: as he puts it, his plumbing isn’t what it used to be. But he maintains a sense of humor. He talks about the nurses who take care of him and says that he likes to joke with them.
“They feel bad for everyone that has to be treated,” he says. “When I kid around, you get a rapport with them, you become friends.”
Pancreatic cancer can occur in two forms: one attacks the part of the pancreas that creates enzymes which make regulatory hormones, like insulin to control glucose levels in blood, explains Dr. Steven Libutti, director of the Montefiore-Einstein Center for Cancer Care. This cancer is called pancreatic neuroendocrine cancer. This is is the kind of cancer that Ron has. The second form of pancreatic cancer is called pancreatic adenocarcinoma, which attacks the part of the pancreas responsible for helping the body digest foods. Adenocarcinoma occurs more frequently and is more deadly.
“Life expectancy for pancreatic adenocarcinomas is often measured in months whereas life expectancy for pancreatic neuroendocrine carcinoma can be measured in years,” Libutti said.
Libutti , who is also associate director for clinical services at the Albert Einstein Cancer Center, says that although pancreatic neuroendocrine cancer is less prevalent, it is increasing.
“Part of it may be we have better means of diagnosing or detecting them and part of it may be that they actually are increasing in incidence,” Libutti said.
The National Cancer Institute estimates that in 2010, there were approximately 43,000 new cases of pancreatic cancer in the United States. That same year, there were 36,800 deaths by pancreatic cancer in the U.S. The data was not split between the two types of pancreatic cancers. According to the New York State Department of Health, there were 2,768 cases of pancreatic cancer diagnosed in 2007. That same year in New York, there were 2,280 deaths from pancreatic cancer.
Libutti is heading the most recent venture in cancer treatment and detection at Montefiore and Albert Einstein Cancer Center. Through a partnership with four other institutions in Texas, Libutti and his team applied for a grant from the National Cancer Institute to research the use of nanotechnology to diagnose and treat pancreatic neuroendocrine cancer and ovarian cancer. In September, the team was granted a $16 million, five-year grant to pursue this technology.
Nanoparticles are tiny particles, smaller than the diameter of a human hair. “The idea is that nanomedicines can be engineered to have unique properties that might allow them to help in the development of therapeutics that can be targeted to tumors as opposed to having a general effect on the entire body,” Libutti said.
Imagine a cancer tumor having a zip code, Libutti says. His goal with this research is to design an agent that can read that zip code. Once the agent is injected into the body, it would go directly to the zip code where the tumor lives. Once that is accomplished, the agent can be sent with medicine to kill the tumor or some other substance that would allow doctors to see the tumor more clearly.
Currently, there are various treatment options for people who are diagnosed with pancreatic neuroendocrine cancer: surgery is usually the first option. If a person is not able to have surgery, either due to medical conditions or because the patient chooses not to, other options include octreotide injections or sunitinib pills, both medicines that slow the growth of neuroendocrine tumors. “Traditional chemotherapy doesn’t work for endocrine cancers,” Libutti said.
Libutti points out that the concept for this research is not new. Doctors use iodine, for example, to diagnose and treat thyroid cancer. There isn’t a naturally occurring substance that responds to pancreatic cancer tumors the way iodine does to thyroid cancer. Libutti’s research aims to fill that void by creating something that will serve the same purpose that iodine does for thyroid cancer.
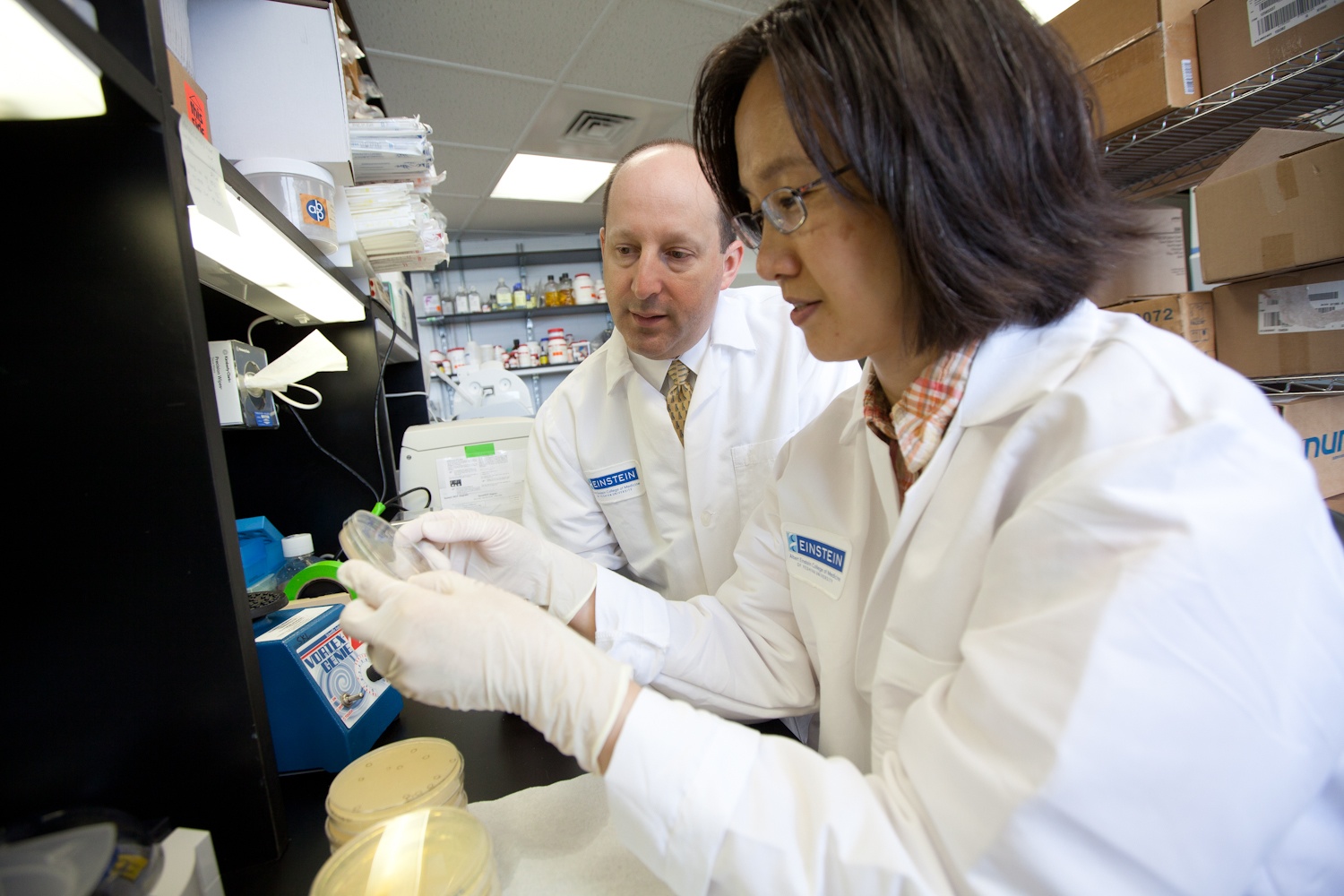
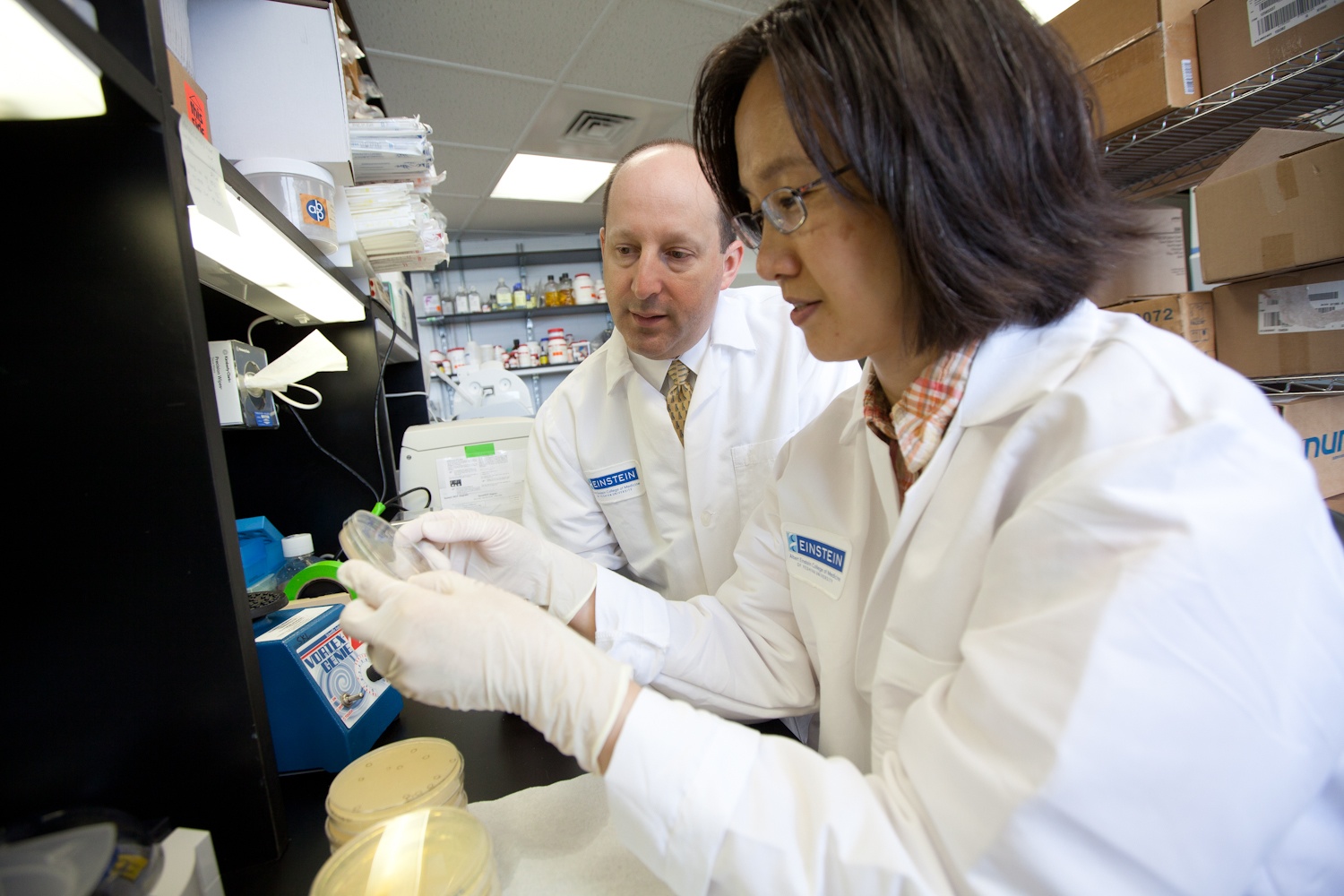
Steven K. Libutti, director of Montefiore-Einstein Center for Cancer Care, is investigating nanoparticles for imaging and treating pancreatic tumors as part of a national five-institution research project funded by the NCI. Pictured in the lab with Dr. Libutti is Mijung Kwon, a senior scientist at Einstein. (Photo Credit: Albert Einstein College of Medicine)
Libutti says that if the research is successful, his team could have a working form of nanomedicine ready to use in seven to ten years. Although the Einstein-Montefiore investigators are focusing on the pancreatic neuroendocrine cancer, the research could produce a substance that would also be useful for pancreatic adenocarcinoma as well as ovarian cancer. These cancers are not linked but they were chosen because of the expertise and interests of the investigating teams.
“My question would be, is this something that they’d be able to detect early?” asked Kristen Angell, affiliate coordinator at the Pancreatic Cancer Action Network’s chapter in Connecticut. Angell’s father was diagnosed with the deadly pancreatic adenocarcinoma in April of last year and was given a year to live. Angell was her father’s caretaker during the last year of his life and says that early detection of adenocarcinoma is crucial to fighting this disease.
Angell points to the progress that’s been made in breast cancer and says she hopes the same efforts can be directed towards pancreatic cancer.
In the meantime, Ron continues his treatment with Dr. Libutti. Although he hadn’t felt too much pain in the beginning, he says he recently started getting an ache on the right side of his body, which he hopes to address with the nurse the next time he is at the hospital. Ron’s pancreatic tumors have spread to his liver, and while the treatment is meant to slow their growth, it is too early to tell what, if any progress has been made.
Since October 2010, Ron has been going to Montefiore for blood work every two weeks, a shot every month, and periodic CAT scans. Having survived a heart attack, prostate cancer seventeen years ago, and now living with a pacemaker, Ron simply did not think that he could survive a major cancer surgery and opted for the second treatment option of monthly injections that slow the growth of the cancerous tumors.
“I’m like an old car,” he jokes.
Ron has found ways to cope with his health: he maintains a strict diet, donates to children’s organizations and prays.
“I got to church a lot,” Ron says, “more so in the last couple of years when my health started deteriorating. I’ve lived my life. I want to live more but it’s in God’s hands.”
(Click on the interactive below to see pancreatic cancer cases and deaths for all five New York boroughs from 1976 to 2007.)